Design thinking in healthcare: design the change, not just the solution
Since 2014, 8D has guided dozens of innovation projects within the healthcare sector. Time and again, we’ve found that design thinking is a powerful approach for untangling complex challenges and creating human-centered solutions. Yet, while the method is now widely used to develop healthcare innovations, we’ve noticed that design-led thinking often comes to a halt at a crucial phase: implementation. In this article, we share insights drawn from a decade of practical experience and research, with one central message: don’t just design the product, design the change itself.
The power of design thinking in healthcare innovation
Design thinking has firmly established itself in recent years as a leading approach to innovation in domains where human behavior, lived experience, and context play a central role. Unlike linear innovation models, design thinking allows space for empathy, co-creation, and iteration; all essential qualities in healthcare settings. Unsurprisingly, more and more healthcare organizations are embracing approaches that involve end users from the start of the design process.
However, this involvement often disappears once the prototype is complete. Human-centered design tends to be strong during the creation phase but drops off when it’s time to embed the innovation into daily practice. It’s precisely in this transition from concept to reality that the biggest challenges arise, and these rarely get solved with a manual or rollout plan alone.
Co-creation shouldn’t end at the prototype
One of the most common pitfalls in healthcare innovation is ending co-creation once the development process is complete. Patients and healthcare professionals are typically involved early on, but as soon as practical questions emerge – such as “How will this fit into our busy workflow?” or “How do we explain this to patients?” – those same end users are often no longer at the table. And yet, they are the key to successful implementation.
Design thinking can offer powerful tools during this phase as well. By applying the same principles (listening, iterating, and creating solutions together) to communication, training, and workflow design, we can generate solutions that are not only effective in transferring knowledge and skills, but also widely embraced by the people that can benefit from them. In this way, implementation becomes not an afterthought, but an integral part of the design process.
Learning from practice
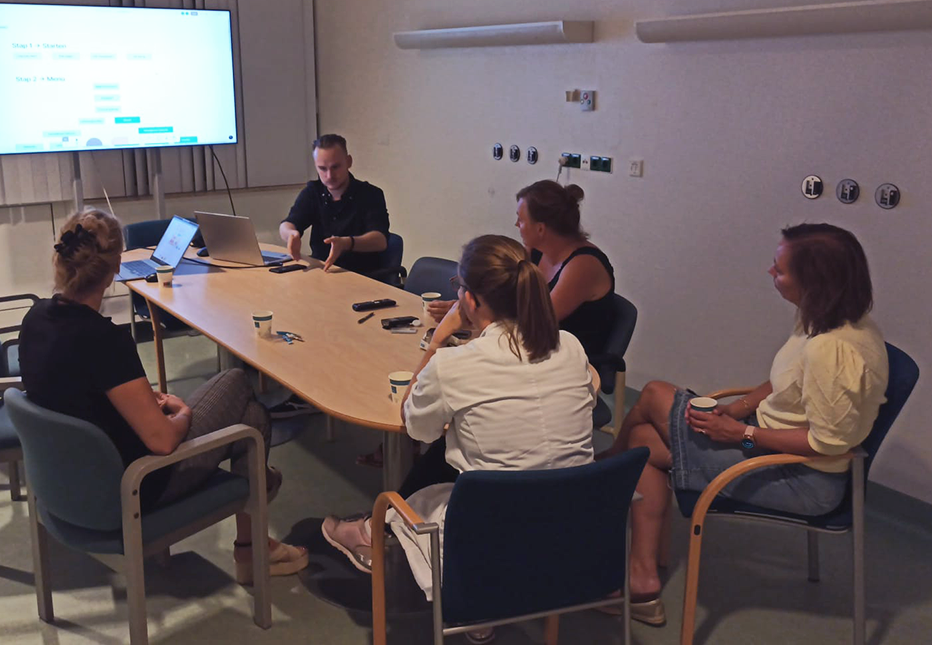
In recent years, our team has made it a point to integrate implementation considerations early in the innovation process and to actively engage our project partners in thinking about this aspect. We’ve also seen more and more partners take inspiring approaches to implementation. Take, for example, the way Frisius MC (formerly Medical Center Leeuwarden) handled the implementation of a walking route on the cardiology ward. Although the route had been designed and physically installed in the building, that didn’t automatically mean that staff and volunteers were actively using it. That’s why the hospital, with guidance from our design team, initiated a co-creative follow-up: together with volunteers, they explored how the route could be introduced to patients, how guidance could be provided, and what concerns or barriers (such as safety or scanning QR codes) needed to be addressed.
These kinds of sessions often yield outcomes that no designer or manager could have developed without input from those working on the ground. Sometimes, the solution is as simple as printing an A4 instruction sheet and placing it on a fridge in the staff break room, or creating a moderated WhatsApp group. In other words, co-creation requires an initial investment in terms of taking the time to discuss things thoroughly, but the solutions that arise tend to be much simpler and more effective in the long run.
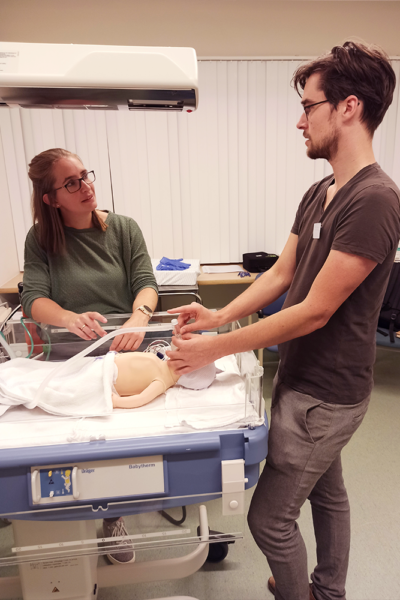
A compelling example from our white paper on healthcare innovation implementation involves intensivist Carina Bethlehem, with whom we collaborated on a VR training program for ICU rehabilitation. On her unit, a “super user” is designated for each new process or tool: a healthcare professional who understands the innovation in depth and serves as a first point of contact for colleagues. No thick manuals – just a familiar face you can quickly approach with a question.
Reflections for policymakers and researchers
If we truly want to use design thinking to enable sustainable innovation in healthcare, we need to broaden our perspective. Researchers must be willing to adopt methods that embrace complexity and context. Think of approaches like investigative rehearsal or embedded trial-and-error. Methods where the process is as important as the outcome. We’re seeing growing openness to these forms of inquiry, but funding mechanisms are still poorly suited to them, with a strong emphasis on guaranteed deliverables. Under such constraints, meaningful design thinking becomes almost impossible.
For policymakers and funders, this means it’s time to rethink how healthcare innovation is financed. The gap between delivery and validation – the infamous “funding valley of death” – is often too wide. Innovations must be in use for years before they gain scientific recognition and qualify for reimbursement. While that requirement is understandable, for many small design agencies and developers (often SMEs) the period in between is financially untenable. Without structural support for implementation and further development, even the most promising innovations are likely to stall in the pilot phase.
Final thought: design the change, not just the solution
The core of design thinking has always been human-centeredness. That focus shouldn’t stop at the prototype but should extend into implementation, training, and embedding. It must also shape how designers collaborate with researchers, and how funders and policymakers create the conditions for change. This means truly listening to where other actors in the innovation ecosystem encounter obstacles. And moreover, responding with empathy and genuine engagement to initiate changes that reach beyond one’s own domain. In the hectic pace of daily life and the pressure to perform, we often lose sight of this. But if we want healthcare innovations to truly take root, we must not only design the applications – we must also design the change itself, systemically. That’s where the real key to sustainable healthcare innovation lies.
TechTalk #1: PhD researcher Lise Beumeler
So who are these people who build bridges between science, technology and social issues? That is what we will be asking a number of partners in the near future. Lise Beumeler – PhD researcher at
RuG Campus Fryslân – kicks off the interview.
Read blog