Shaping the training and its implementation
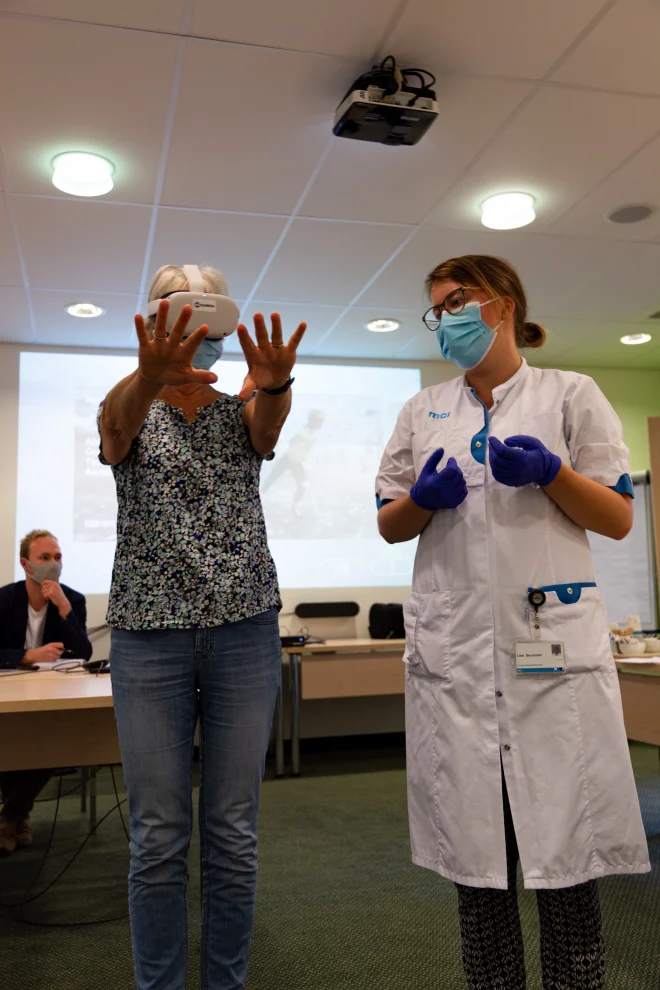
Early in the co-creation process, it became clear that the training should not become a traditional standalone e-learning. Dijkman: “E-learning alone often doesn’t give nurses enough support to put new knowledge into practice. Ideally, you want to apply new skills directly on the work floor, in everyday situations. The challenge is that it also has to fit into an already busy schedule without adding pressure.”
Participants expressed enthusiasm for learning together and raised important implementation questions. “Some departments have a fixed moment each day when they can pause for training, others don’t,” says Dijkman. “If we wanted something truly department-agnostic, we had to take that into account: no long instructions or meetings, but a format you can use quickly and easily.”
When the needs and conditions became clear, 8D was brought in to translate “ideas and requirements” into a tangible product. “By then we knew we wanted to create short, practice-based assignments that nurses could complete throughout the day,” Dijkman says, “but we still had to figure out how to offer those assignments in a low-threshold way.”
“We knew we wanted to create short, practice-based assignments that nurses could complete throughout the day, but we still had to figure out how to offer those assignments in a low-threshold way.”
From idea to product
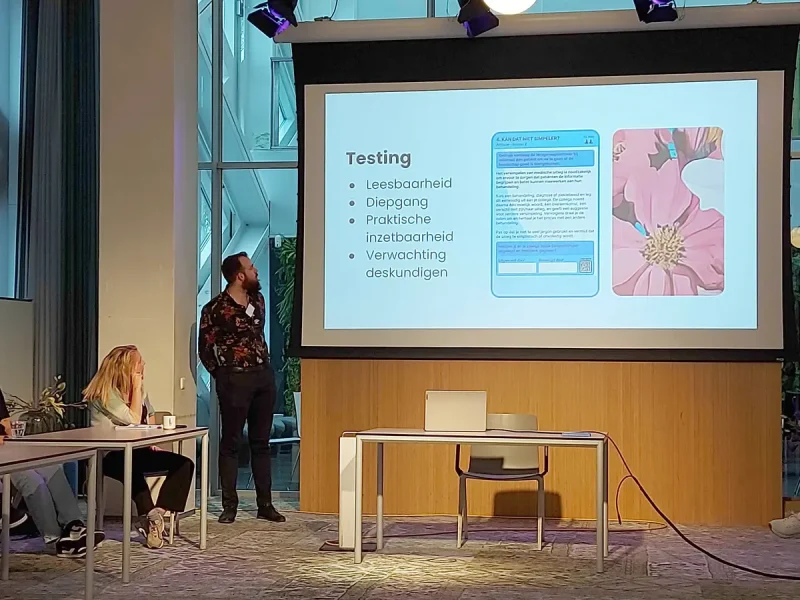
Gradually, the idea of a card set emerged. A seemingly simple format that turned out to involve many design choices. Questions arose such as: What size works best? How long can the texts be while remaining usable? Should additional information be available, and if so, how do we make it accessible? How can we add a playful element without requiring extensive instructions or team meetings?
8D designer Giel Hekkert helped map out these choices. “By showing different prototypes of the cards, the co-creation group could make well-informed decisions,” he explains. “Prototyping forces you to think concretely about your goals, your users and the context in which the product will be used. That is the essence of strategic design: you consider the entire system around the product.”
This phase also revealed new constraints. The challenge was to create one design that could work both in education and in the hospital, something that proved nearly impossible once the content and depth were explored. Lankhorst explains: “Students need to practise the same principles, but at a level and in a context suited to their stage of learning. And the practice itself differs: students practise mostly with one another, while nurses work with real patients in established teams. That requires different content and a different dynamic.”
This tension sparked the idea not to create one fixed product but a flexible framework. Hekkert: “We designed a base template and guidelines that allow users to create new cards or adaptations themselves. Not a static product, but a foundation that departments, researchers and educators can build on. This way they do not need to return to us for every small change, saving time, energy and budget for research and implementation.”
“Prototyping forces you to think concretely about your goals, your users and the context in which the product will be used.
Testing and building support
Two versions of the card set have now been fully developed with practical assignments: one for use in hospitals and one for use in education. Examples include: applying the teach-back method with a patient, or logging into the digital patient portal together. Once completed, the cards can be placed on the team board in the correct spot, gradually forming a picture that colleagues complete together. Each card includes a QR code linking to additional information.
“It was wonderful to see how enthusiastic participants were when creating assignments and supporting materials,” says Lankhorst. “The content now aligns closely with what they encounter in their daily work.”
In the coming period, the card sets will be tested in both settings. In the hospital, Dijkman is studying how the assignments affect nurses’ skills and attitudes and their communication with patients. In vocational education, the focus is on strengthening students’ knowledge and awareness. According to Lankhorst, the motivation to participate is high. “Participants who joined the earlier co-creation sessions are now genuinely excited to start using the cards.”
Hekkert finds that remarkable: “We often hear how difficult it is to find enough engaged participants for evaluation. The time invested in co-creation is now paying off through stronger support and genuine willingness to use the product.”
Ambitions for the future
Dijkman hopes the training will ultimately make a tangible difference. “If nurses can more quickly recognize when someone needs extra explanation, or feel more confident exploring digital tools together, that contributes to better care. Ideally, we would eventually see a decrease in things like medication errors or readmissions because professionals offer better support to patients who struggle to access and understand healthcare information. This project is our contribution to making that possible.”
She also sees opportunities for broader application of this learning approach. “There is a lot of interest from other departments and colleagues, and people are already exploring how this method could work in different contexts. If the approach proves effective, we will have a powerful example of how to support learning on the work floor in a simple and accessible way.”
Empowering Nurses to Empower their Patients (ENEP) is a collaboration between Isala, Windesheim University of Applied Sciences, University of Twente, Drenthe College, Pharos and 8D | Research + Design = Impact. The project is funded by ZonMw.